From Story to Strategy: Bringing Patient Voices into Medical Education
A Smart Patients practical guide for educators who want to make continuing education more human, evidence-based, and effective.
“Smart Patients is an online health community serving 100s of different patient communities. We primarily provide a means for patients and their families to learn about illnesses, to seek and offer social support, and to connect with others in similar circumstances. We also help with “the wisdom of the crowd”.
Additionally, benefits are seen within specific illnesses, and are most beneficial for certain individuals, and would be otherwise unattainable outside of the context of online health communities. increased disease knowledge can help patients make more informed decisions about their health.”
- Written by a Smart Patient community member
Why Patient Voice Matters
Medical education is evolving. Clinicians learn not just from guidelines, but from real lives. When patients share their experiences inside continuing professional development (CPD) and continuing medical education (CME), it changes what healthcare professionals remember, how they empathize, and ultimately, how they practice.
“We believe patient voice adds more than feeling; it adds real-world evidence drawn from experience.”
Research consistently shows that including patients in education:
Increases empathy and knowledge retention among HCPs
Strengthens adherence to best practices
Improves shared decision-making and patient confidence
Builds trust between providers and the people they serve
It’s time to make that practical—so every educational activity can benefit.
From Story to Strategy
At Smart Patients, we see thousands of conversations unfold every day between people living with serious conditions and those who care for them. Their stories reveal patterns, barriers, and teachable moments that can power better education.
When we integrate these voices into medical learning, clinicians gain context. Instead of just learning what to do, they understand why it matters.
“As we often say at Smart Patients, ‘When patients are invited as partners, education becomes a dialogue, not a download.’”
Four Steps to Integrate Patient Voice
1. Identify & Recruit
Define the purpose: are you addressing empathy, disparities, or practical communication gaps? Find the right partners—patients, advocates, or caregivers—whose experiences align with the program goals.
2. Prepare & Orient
Transparency builds confidence. Share learning objectives, timelines, and expectations early. Discuss compensation, disclosures, and accessibility needs.
3. Partner & Co-Design
Include patients from the start. Rehearse together. Give them a voice in shaping tone, focus, and format so their perspective lands with purpose.
4. Measure & Sustain
Track more than satisfaction. Measure empathy, trust, or intent-to-change among learners—and share those results with your patient partners. Partnerships that close the feedback loop are the ones that last.
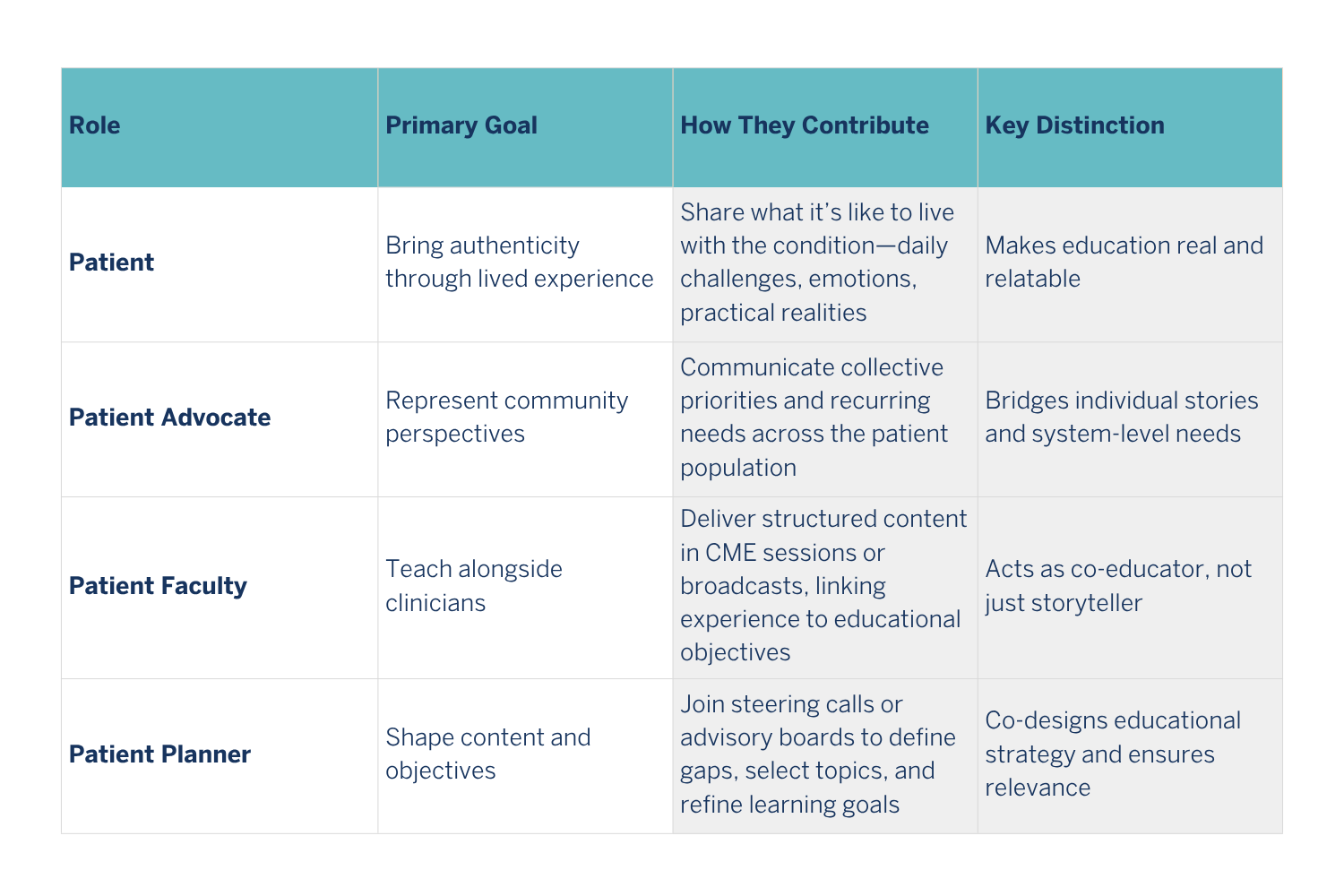
Roles That Make It Work
Every successful program depends on choosing the right kind of partnership. Patients can contribute in different ways depending on the goals of the activity—whether that’s bringing authentic stories, representing a community, co-teaching alongside clinicians, or helping design the curriculum itself.
These roles build on one another to move education from story to strategy.
Patients bring education to life in different ways. Some share their lived experience, making learning real and relatable. Others represent their communities, connecting individual stories to system-level needs. Many teach alongside clinicians as co-educators, while others help shape goals and content to ensure education stays relevant to what truly matters.
Quality and Ethics in Practice
Inviting patients into education is only meaningful if it’s done well. Clear expectations, fair recognition, and ongoing respect are what turn a single collaboration into a long-term partnership. These principles keep patient engagement authentic, ethical, and sustainable.
Patient partnerships work best when they’re grounded in respect.
Parity: Compensate fairly; recognize contributions equally.
Transparency: Be clear about roles and disclosures.
Preparation: Offer orientation and plain-language materials.
Feedback: Share program results back with participants.
Sustainability: Rotate diverse voices, maintain relationships.
Ethical engagement turns a single invitation into a sustainable learning culture
Proof in Practice: A Case Study
In one Smart Patients focus group, women living with gynecologic cancers described feeling unprepared to discuss molecular testing or treatment side effects. Educators turned those verbatim insights into a CME module for oncologists focused on communication and individualized therapy. Six months later, learners reported greater confidence in discussing molecular testing and improved patient satisfaction scores.
A simple shift—from assuming to asking—changed clinical conversations.
Start Small, Start Real
You don’t need a new department or a big budget to do this well. Start with one module, one advisory meeting, or one patient panel. Invite one patient to review slides, co-present, or share a recorded reflection. Each conversation deepens understanding—and every shared story has the power to change practice.
Every time a patient helps teach, healthcare learns how to listen. Patients are powerful teachers, and when education is centered around their lived experience, the whole system improves.
About Smart Patients
Smart Patients partners with educators, clinicians, and life-science organizations to bring lived experience into continuing education and life sciences decision-making. Through moderated online communities, focus groups, and patient-faculty programs, we help transform stories into strategies for better care.
References
Accreditation Council for Continuing Medical Education. The Patient Partner Roadmap: Fostering Meaningful Partnerships in Continuing Education. 2024.
Greene J, et al. Patient Preferences and Adherence. 2015.
Hibbard JH, et al. Health Affairs. 2004; 23(2): 216-226.